Can AI-driven robotics be trusted for elderly care and palliative medicine?

Can AI-driven robotics be trusted for elderly care and palliative medicine?
by Nathaniel 10:31am Feb 01, 2025

Can AI-driven robotics be trusted for elderly care and palliative medicine?
AI-driven robotics has shown great promise in transforming elderly care and palliative medicine by offering solutions that improve the quality of life, enhance safety, and provide more efficient care. However, whether such systems can be trusted in these sensitive and critical areas requires careful consideration of several factors, including reliability, emotional engagement, ethical concerns, and the nature of care provided. Below are the key factors influencing the trustworthiness of AI-driven robotics for elderly care and palliative medicine.
1. Emotional and Social Engagement
One of the most critical aspects of elderly care and palliative medicine is the emotional and social needs of patients. Elderly individuals, particularly those in palliative care, often face loneliness, depression, and a desire for companionship. AI-driven robots, such as social robots designed to engage with patients, can provide companionship, help alleviate loneliness, and even support basic emotional needs. However, these robots do not possess genuine emotional intelligence and cannot form the authentic bonds that human caregivers or family members can provide.
Challenges:
Lack of True Empathy:While AI robots can simulate conversations and react to emotional cues, they lack the capacity for true empathy, which is vital for building trust and providing emotional support in palliative and elderly care settings.
Social Isolation:Relying on robots for social interaction could potentially deepen feelings of isolation, particularly if patients come to depend on machines for emotional support rather than human connections.
Trust Considerations:
Many elderly patients, especially those in end-of-life care, may prefer human contact to robotic interaction. While AI-driven robots can be beneficial in some contexts, they should not be viewed as a replacement for human caregivers who can offer genuine empathy and social engagement.
2. Medical Safety and Precision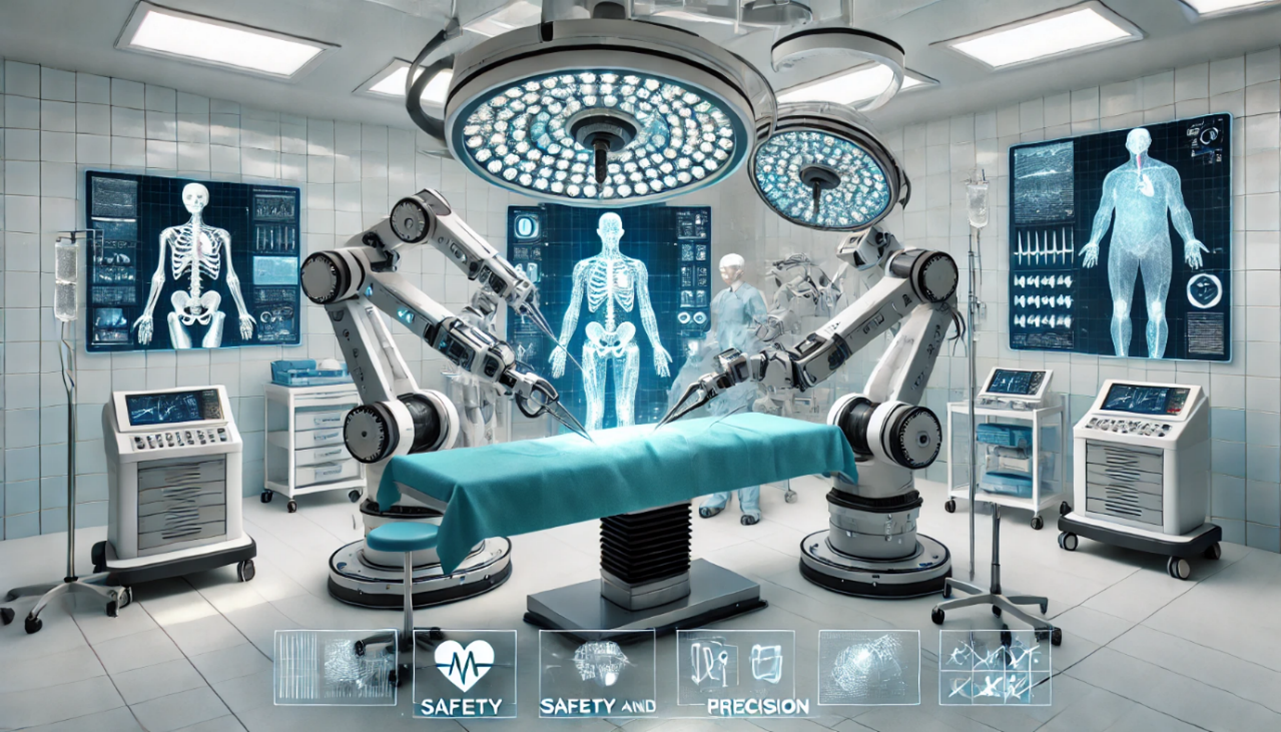
In elderly care and palliative medicine, medical safety is paramount. AI-driven robotics can play a role in monitoring vital signs, administering medications, and assisting with mobility. Robots designed for healthcare tasks can provide precise, consistent, and timely interventions that enhance safety and reduce human error.
Examples:
Medication Assistance:Robots can be equipped with sensors and algorithms to monitor medication adherence, remind patients to take medications, and even dispense drugs with great accuracy.
Fall Prevention:Robotic systems can monitor a patient’s movements and provide assistance with walking, reducing the risk of falls a major concern in elderly care.
Challenges:
Technical Reliability:AI systems and robots must be highly reliable, as failure in critical situations (e.g., administering wrong medication or missing a medical emergency) could have severe consequences. Trust in these systems depends on their performance, consistency, and failure rates.
Emergency Situations:AI systems may not be prepared to handle unexpected medical situations in the way human caregivers or doctors can. While robots can monitor patient conditions, their ability to make complex decisions or respond to sudden changes in health status remains limited.
Trust Considerations:
Elderly patients and their families may feel more comfortable with human caregivers who can react flexibly to changes in medical conditions, as opposed to robotic systems that follow predetermined algorithms.
AI and robots can assist in routine tasks, but their role should be viewed as complementary to human caregivers rather than a replacement.
3. Ethical and Privacy Concerns
AI-driven robotics in elderly care and palliative medicine raises ethical concerns, particularly related to privacy, consent, and data security. Many AI systems are designed to collect and process sensitive personal health data, which can lead to concerns about how this information is used and who has access to it.
Challenges:
Informed Consent:Patients, especially those with cognitive impairments such as dementia, may not be able to provide informed consent regarding the use of AI-driven robotic systems. Ensuring that these patients and their families understand the technology and its risks is a crucial issue.
Data Privacy:AI-driven robots often collect data related to a patient’s daily activities, health metrics, and personal interactions. Ensuring this data is secure and used ethically is essential to maintaining trust in these systems.
Potential for Exploitation: There are concerns about how companies might use sensitive health data for profit or how AI systems might be employed in ways that prioritize cost savings over patient well-being.
Trust Considerations:
Transparent policies regarding data collection,storage, and usage are necessary to build trust with patients and their families.
Clear guidelines on consent and privacy protections should be established, particularly when dealing with elderly individuals who may have diminished capacity to understand the implications of data collection.
4. Personalization and Adaptability
Elderly care often requires highly individualized care plans that account for physical, cognitive, and emotional needs. AI-driven robotics can be designed to assist with tasks tailored to individual needs, but there are challenges regarding their ability to adapt to the wide variability in patient conditions.
Challenges:
Personalization of Care: AI-driven robots must be capable of adapting to the unique health conditions and preferences of each elderly patient. A “one-size-fits-all” approach may not work, especially in palliative care,where the focus is on comfort and quality of life.
Cognitive Decline:Many elderly individuals, particularly those in palliative care, suffer from cognitive impairments such as dementia. While robots can be programmed to assist with daily tasks, they may struggle to effectively communicate with or support patients with severe cognitive decline.
Context Awareness:Robots may have difficulty recognizing subtle changes in a patient’s condition that are not directly related to physical health metrics. For example, they may not fully understand or respond to emotional shifts or signs of distress in the same way a human caregiver can.
Trust Considerations:
Trust in AI-driven robots in elderly care will depend on their ability to provide highly personalized care and adapt to changing health conditions over time. While robots can help with tasks like medication management and mobility support, their limitations in understanding the full context of a patient’s needs may affect their role in palliative care.
5. Cost and Accessibility Cost and Accessibility
Another limitation of AI-driven robotics in elderly care and palliative medicine is the cost of implementing and maintaining such systems. These technologies can be expensive, and the financial barriers may limit their widespread adoption, particularly in low-income settings or for families without sufficient resources.
Challenges:
High Initial Investment: The upfront cost of AI-driven robotic systems can be prohibitive for many families and healthcare providers, especially in private home care settings.
Maintenance and Support: Ongoing maintenance, software updates, and troubleshooting are required to ensure that robots continue to function properly. This adds to the cost burden and may require specialized knowledge or training to manage effectively.
Trust Considerations:
The accessibility of these technologies will influence how trusted they are in elderly care. If robots are perceived as a luxury or an expensive alternative to human caregivers, there may be skepticism regarding their widespread use, especially when human touch and connectionare seen as essential to quality care.
6. Human Oversight and Accountability
Robotic systems in elderly care and palliative medicine should not operate in isolation. Human oversight is crucial to ensure that the technology is used appropriately and that any shortcomings or errors are promptly addressed.
Challenges:
Supervision: AI-driven robots must be monitored and supervised by human caregivers to ensure that they do not make errors or overlook important patient needs.
Accountability:If something goes wrong (for example, if a robot misses an emergency or administers incorrect medication), it can be difficult to determine who is responsible the healthcare provider, the robot’s manufacturer, or the patient’s family. Establishing clear accountability frameworks is essential.
Trust Considerations:
Patients and their families must feel confident that human caregivers are overseeing AI-driven robots to ensure their safety and well-being. Robots should act as assistants to human professionals rather than replacing them entirely.